
Most women with breast cancer, or even those with a high risk of developing breast cancer, will have some type of surgery as part of their treatment plan. The type of surgery recommended will depend on the location and size of the tumor, medical history, and other factors.
There are two main types of surgery to remove breast cancer: lumpectomy and mastectomy.
Lumpectomy is the surgical removal of a lump from the breast while preserving the rest of the breast and nipple. It is generally followed by radiation for most types of breast cancer.
Mastectomy is a surgery in which the entire breast is removed, including all of the breast tissue and sometimes other nearby tissues. There are several different types of mastectomies. Some women may also need to have both breasts removed; this is called a double mastectomy.
Both mastectomy and lumpectomy are equal in terms of survival and long-term outcomes from the cancer perspective; for both options, lymph nodes may need to be removed. The choice of whether to use chemotherapy (IV or oral drugs) to help improve the survival is not dependent on which surgery is chosen. That is an independent decision that relates to the biology of the cancer and not to how it is removed.
Mastectomy may be a preferred option for women who:
Patients at the Rochester Regional Health Breast Center of Excellence may be referred by their primary care provider or OBGYN, but patients can also self-refer – meaning they don’t need a referral from another provider after their breast cancer diagnosis.
Once a patient arrives at their first appointment, they have a consultation with their surgical team to discuss which type of surgery they will undergo, breast reconstruction options to restore the appearance of their breasts, and any other surgical guidance. If breast reconstruction is desired, the patient will meet with a plastic surgery team as well. A date or multiple dates for surgery will then be scheduled.
Reconstructive procedures are generally covered by insurers as part of the cancer treatment and not as a cosmetic approach. For women who decide not to have their breast reconstructed, there are options for bras and fitted forms that may also be of interest.
Breast care nurse navigators will work with each patient to help them through the various stages of care so there is less pressure on the patient to make calls and set up appointments during this stressful time in their life.
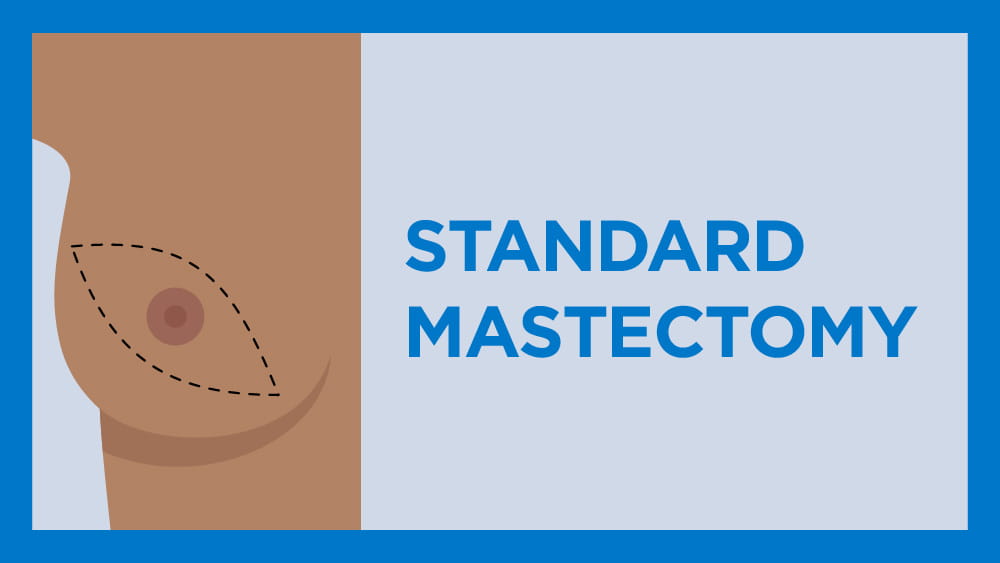
A standard mastectomy surgery involves the removal of the nipple, areola, and breast tissue. Lymph nodes to which the cancer has spread are also removed – unless the mastectomy is for preventative reasons.
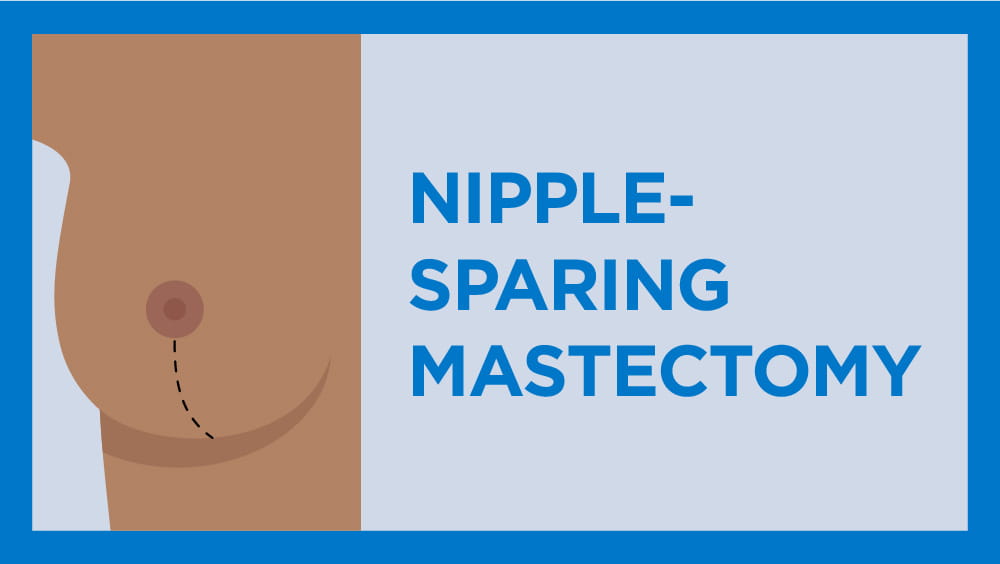
An alternative surgery called a “nipple-sparing mastectomy” leaves the nipple and skin intact on the breast, but removes the breast tissue. In certain cases, depending on breast anatomy, this can be performed as an alternative. However, there will not be any sensation left in the nipple.
In total, a mastectomy takes approximately 1-3 hours to complete. This may vary based on breast size, the removal of one or both breasts, and the patient’s decision for breast reconstruction.
Once the surgery is complete, patients have the option to stay in the hospital overnight or to go home on the same day as long as the provider ensures they are stable and properly trained for post-operative care. Most patients are able to return home on the same day, according to Dr. Medeiros.
“For patients heading home on the same day, we want to make sure they know how to care for themselves before they leave,” Dr. Medeiros said. “We teach them about proper pain management and how to drain fluid from the surgical site – through both direct conversation and video learning.”
Within one week of surgery, women are able to do most normal daily activities with some modifications. Patients are encouraged to use their arms normally and work toward regaining their full range of motion as they are comfortable. Recovery time may be longer if breast reconstruction was also done.
Doctors strongly encourage patients to remain out of work for about six weeks so they can resume all normal activities without straining their incision and to ensure planning for next steps.
In the days following the surgery, some pain, swelling, and tenderness at the surgery site are to be expected. However, since mastectomy only removes tissue and not muscle, most women do not experience a significant level of pain. Pain can usually be managed with mild pain relievers such as ibuprofen (Advil or Motrin), naproxen (Aleve), or acetaminophen (Tylenol). If the pain is more severe, doctors can prescribe medication as needed.
Patients will have their first post-operative visit about one week after surgery. At this appointment, their provider will discuss the pathology results from the surgery, adjustments to daily activities as needed, and the next stages of care based on the specific type and stage of cancer that was removed.
For some patients, additional treatment may be needed. This can include radiation therapy, chemotherapy, or a combination of both.
If radiation therapy is needed, it typically begins one month after surgery and lasts about three weeks with daily radiation sessions.
“The most important elements of recovering from a mastectomy have less to do with the physical surgery and more to do with the emotional recovery,” Dr. Medeiros said.
With the many patients Dr. Medeiros has seen over the years, she said it takes at least 12 months after treatment for most patients to begin healthily processing the emotional and mental effects of their journey with breast cancer.
“When patients are in the middle of treatment, there is something to focus on,” Dr. Medeiros said. “It is the lull between treatments and tests that prove to be more emotionally challenging.”
Dr. Medeiros has some suggestions for maintaining good emotional health based on her experience with patients and their families.
Keep it simple
Keeping their day-to-day schedule simple will help. Getting through the initial treatments is the most important thing a patient can do for themselves and those around them.
Avoid big changes
A cancer diagnosis leads some patients to want to make significant changes to their lifestyle. Moderate physical exercise can help with stress reduction and eating healthy is a good practice in general. However, making significant lifestyle changes in the middle of rigorous cancer treatment should be avoided as they adjust to their new treatment schedule.
Join a support group
Rochester Regional Health has strong connections to a wide variety of breast cancer support groups and networks within the local community. Some of those organizations include: