
For athletes of all ages, one of the most serious leg and knee injuries is an anterior cruciate ligament (ACL) tear.
An ACL tear often happens in sports with quick stopping and twisting or pivoting motions, such as football, basketball, or soccer – usually with awkward foot landings or changing directions.
With many injuries, the body’s own blood supply provides an injured area with the needed materials to heal on its own. However, the blood that would help the ACL heal runs through the ligament itself, meaning soft tissue cannot heal on its own. When this ligament is torn – either partially or fully – the vast majority of cases require reconstructive surgery with surgeons creating a new ligament for the patient.
Michael Stanton, MD, is an orthopaedic surgeon with Rochester Regional Health, and breaks down the surgery and recovery process.
When an ACL tear initially happens, a patient will typically feel an immediate sharp pain in the knee and rapid swelling in a short period of time. Within a few hours, patients will see a significant amount of swelling.
Within a few days of the injury, the patient is brought to an imaging center where they are evaluated with an X-ray to ensure there are no fractures. This is followed by a magnetic resonance imaging (MRI) scan and a physical exam by a provider to evaluate how much the patient’s knee is shifting.
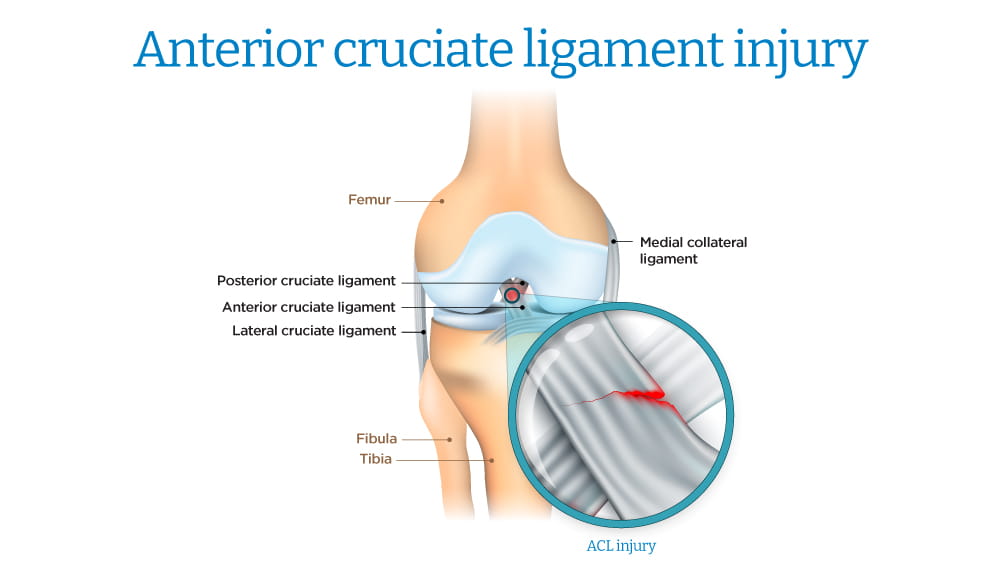
When the ACL is functional, the provider should be able to move a patient’s shin bone forward while the patient is lying down, allowing the shin bone to move a little bit but eventually stop with the ACL pulling tight like a belt snapping to hold the shin in place compared to the thigh bone. If the bone continues to move, this is indicative of an ACL tear.
After deciding to move ahead with reconstructive ACL surgery, the patient will work with the surgeon to determine the source of the tissue graft to build the new ACL. This can come from either a cadaver or the patient’s own body.
On the patient’s own body, the graft can come from a few different areas of the body, including the patellar tendon, hamstring, or quadricep. Research shows younger athletes have a lower risk of tearing their ACL again if they use their own tissue during a graft. Once a patient is in their mid-30s, the results of using a cadaver vs. a patient’s own tissue are roughly the same.
“Choosing the correct tissue for a graft is important to have the best possible result,” Dr. Stanton said. “Some patients are concerned about taking tissue from their own body and want to know about any long-term consequences. Physicians educate each patient to help them make the best decision that leads to the best possible outcome.”
Most procedures are performed at outpatient surgical centers. The surgical team will consist of a surgeon, anesthesiologist, physician assistant, nurse, and surgical technologist.
Patients will be placed under general anesthesia for the procedure and receive a nerve block that is in place for about 24 hours. Once a patient is fully under anesthesia, the surgery takes 60-90 minutes and is performed arthroscopically.
The surgeon needs to drill holes through the shin and thigh bones in order to accurately place the ACL graft. Once in place, the graft is held in place with screws, buttons, or other devices, according to the American Academy of Orthopaedic Surgeons.
Patients will have a scar running along the area of their leg where the graft is sourced – most commonly along the front of their knee at the patellar tendon.
Regaining full function of the ACL is a long process. It can take 7-8 months for a patient with an ACL tear to fully recover to the point where they are playing their sport without any movement restrictions.
In the first few days after surgery, there is some discomfort. Most patients will manage any pain with anti-inflammatory medications or low-dose narcotics. Medication is typically no longer needed one week after surgery.
“We want to manage their pain enough that they feel comfortable to do their range of motion exercises after surgery,” Dr. Stanton said.
Patients will start with physical therapy exercises to build up their range of motion within one week of their surgery. Goals vary for each patient, but the overall aim is to reduce the patient’s pain and swelling while improving their range of motion and getting them back to everything they want to do in an athletic setting.
Most patients will use crutches or other mobility aids for 2-3 weeks after surgery to help them move around. Over time, physical therapy will help them:
As long as patients follow their physical therapist’s guidance, they can avoid a build-up of scar tissue deep within the knee. Research shows accumulating scar tissue can reduce range of motion and lead to weaker leg muscles if left untreated.
Most surgeons will have patients wear an ACL brace in the first 12 months after they return to athletics. The brace provides support for the knee but does not help to heal the injury – which is why athletes are unable to keep playing with a brace when they have the ACL injury.
From the initial surgery, a graft can take up to 18 months to gain its full strength and function as a new ACL. This is what makes the brace so strongly encouraged by surgeons.
“While it is unfortunate that these injuries are common, it can be helpful for most patients to know they are not the first person to go through this,” Dr. Stanton said. “This surgery is performed by doctors who do quite a few of these procedures. Having someone who is confident in their technique is very important because it can affect the future outcomes of these patients.”