To help patients navigate serious and life-threatening illnesses, health care workers offer different types of medical care – including hospice and palliative care.
For people who are not familiar with these two forms of care, they may seem very similar. Stephanie Coco is a hospice and palliative care social worker through Rochester Regional Health Home Care and explains how the two types of care are related and how they differ.
Hospice care is a program for individuals who are living with a life-threatening or terminal illness that gives them a prognosis of six months or less to live. These individuals are focused on comfort and quality of life, rather than healing measures.
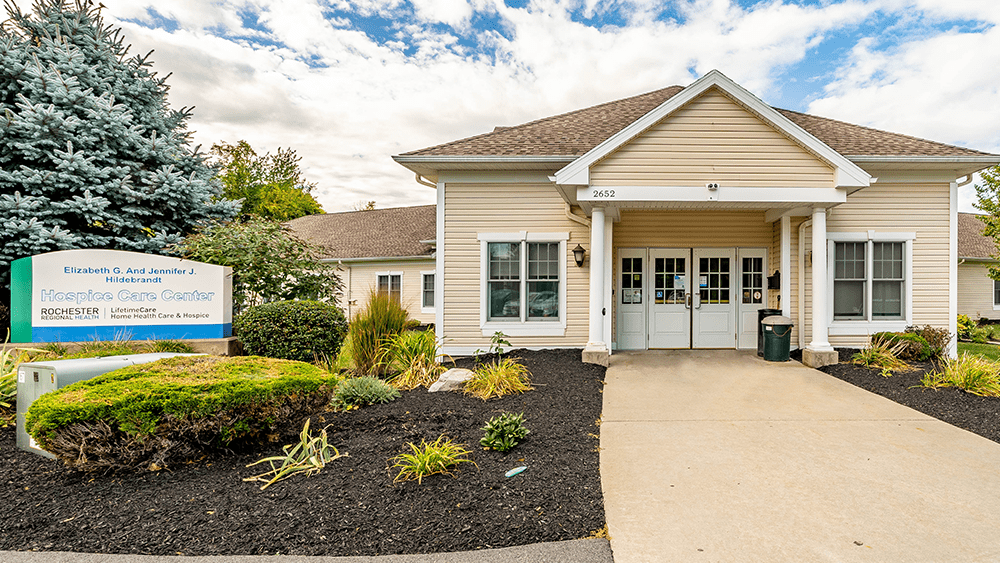
Through hospice care, individuals are given supportive care wherever they are – at their home, or in an assisted living facility, comfort care home, nursing home, hospital, or hospice facility. Hospice care teams provide comfort using a variety of therapies and services with the goal of meeting the physical, emotional, and spiritual needs of patients and their families.
Hospice care teams are interdisciplinary and bring together different areas of health care expertise to provide comfort measures for patients who need end-of-life care. Each team has an attending physician, medical director, nurse, and social worker who provide primary care and support to a patient and their family.
Depending on the needs and wishes of the patient and family, other team members may include:
Palliative care is for individuals living with a life-threatening or serious illness (e.g., cancer) who do not meet the prognostic criteria for hospice care and/or still want to continue with treatment.
“Perhaps a cancer patient is told by their provider that they have a 4-month prognosis but have the option to continue treatment,” Coco said. “If they want to pursue that treatment, we would fully support their decision with a palliative care approach.”
Similar to hospice care, a palliative care team usually consists of a nurse and social worker working together, with other providers available as needed. This may include therapists (physical, occupational, speech) or home health aides. Each of these team members will report back to a doctor about a patient’s progress and their needs.
“Team members work closely together in hospice and palliative care,” Coco said. “Nurses and social workers visit patients together as much as possible so that the physical, emotional, and logistical parts of the patient’s care are addressed. Family members, patients, and providers can bounce questions off of one another, creating a truly comprehensive approach to care.
Once a patient is assessed and deemed eligible for hospice care, the patient is provided with a comfort kit of medications. The kit contains a small number of medications to help patients experiencing common symptoms seen at end of life: anxiety, pain, restlessness, nausea, shortness of breath, or agitation. These medications are provided through hospice care at no additional cost.
Durable medical supplies and equipment such as a hospital bed, walker, wheelchair, or incontinence supplies are also provided through hospice care at no additional cost.
Since the focus of hospice care is to provide comfort measures, hospice care staff do not bring in rehabilitative therapies (physical, occupational, speech), provide diagnostic imaging, or use other forms of care that would prolong a patient’s life.
Hospice care services are not provided at a patient’s home on a 24/7 basis. A hospice team member will be available by phone in case of emergencies. This is explained to the patient and their family before hospice care begins, since it is a common misperception. Together, the hospice care team educates and empowers caregivers to be able to manage a patient’s needs when providers are not at their home.
Many of the services offered through hospice care are offered through palliative care. Like hospice, palliative care focuses on symptom and medication management. Nurses will continually assess patients and collaborate with their medical providers (primary care provider, specialists, etc.) to ease pain, anxiety, and other symptoms. Similar to hospice care, palliative care is available anywhere a patient is living and/or being treated.
Palliative care social workers will also assist in long-term planning to help patients determine what their goals are, work with them as they consider additional treatments or a shift to hospice care, and provide emotional support for patients and their families.
Durable medical equipment (e.g., hospital bed, walker, cane) is not covered through palliative care services. Patients and their families can seek coverage through their medical insurance.
Similar to hospice care, palliative care does not provide 24/7 supervision for patients. However, if a patient is experiencing a health crisis, a palliative care patient may call 911 or go to the hospital for medical evaluation. For hospice care patients, any medical needs or crises will be directed to the hospice team.
“Most services in hospice and palliative care will be covered under Medicare or Medicaid. When a person enters the hospice care program, their insurance stops covering many preventative and curative treatments such as primary care visits, specialists, hospital visits, tests, imaging and other treatments, and starts to cover the many supportive services provided by hospice,” Coco said.
The choice to seek either palliative or hospice care can be a difficult one for patients and their loved ones. When it comes time for an individual to acknowledge a need for hospice services, they may not want those services because it feels like an acknowledgement of how close they are to the end of life.
No matter the decision made by patients and their families, hospice and palliative care teams meet patients wherever they are in their health journey – supporting them as best as they are able.
“Death is a difficult time in many people’s lives,” Coco said. “Some people accept it, but for many, it is a difficult part of life to encounter. If our team can help make that time even a little bit easier for an individual and their family, and help everyone involved feel a little less alone, we want to be there. Our goal is to make a difficult situation better, and while we can’t magically cure anyone of their illness, we can instill hope and let them know they will not be alone in this journey.”