
Having a food allergy can be very challenging – especially for families with children.
Peanut is one of the most common food allergens – affecting as many as 2 percent of all children in the U.S. Without intervention, the vast majority of those children will not outgrow their allergy over time. This can be a tough reality for both parents and children.
In the fall of 2021, Coleen and Andrew stepped into this reality with the birth of their son Jackson.
Coleen and Andrew brought their healthy newborn son home from the hospital and had a fairly typical first child experience with him through the winter months.
As Jackson started reaching his milestones and his parents started feeding him solid foods, Coleen noticed he had a few uncommon reactions. He threw up immediately after trying scrambled eggs for the first time, but she didn’t think much of it.
When she introduced him to small amounts of peanut butter, Coleen said Jackson had no issues the first couple times. Then something changed.
“The next time we tried peanut butter, within a short amount of time, Jackson broke out into hives and got a rash down his chest,” Coleen said.

Coleen’s next phone call was to an allergist, who brought them in for an appointment. After bloodwork and skin tests, Jackson was confirmed to have a peanut allergy – along with allergies to egg, milk, sesame, and certain tree nuts.
“I’m a teacher, so I have experience with students who have peanut allergies,” Coleen said. “That also means I know it’s going to be a lifelong thing.”
Coleen and Andrew decided to talk with their pediatrician about what their next steps would be, given the number of allergies with which Jackson would be living. Their recommendation was to see allergist Shahzad Mustafa, MD, who specializes in allergy and clinical immunology.
From the moment she and her husband met with Dr. Mustafa, Coleen said he was deeply informative and reassuring – pointing to studies and research data showing the progress that young children were able to make with allergy treatments. After analyzing Jackson’s bloodwork and talking through potential options with his parents, Dr. Mustafa was able to create a roadmap for Jackson’s treatment. The goal of their decision-making: boost Jackson’s chances of outgrowing his peanut allergy by the time he went to kindergarten.
“Early on, the phrase ‘life threatening allergy’ was discussed frequently when talking about Jackson and we didn’t have any context for it,” Coleen said. “Dr. Mustafa gave us percentages and more information that helped us feel more comfortable.”
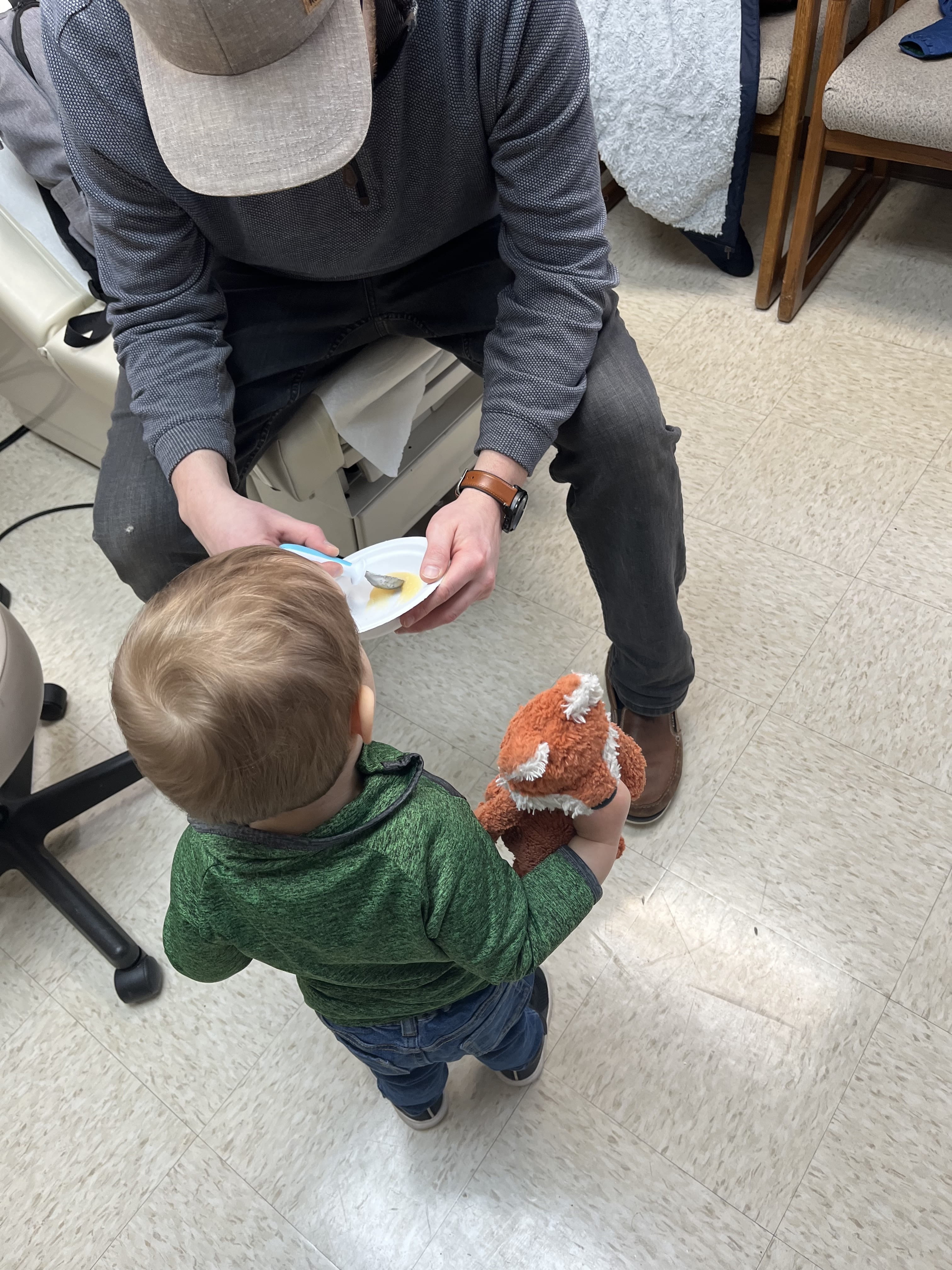
Jackson soon began a therapy called oral immunotherapy (OIT) – a treatment designed to decrease the likelihood of an allergic reaction if exposed to an allergen, and in younger children, potentially facilitate outgrowing the allergy. OIT starts with children as young as 9 months being given a small amount of peanut protein in a supervised setting. If tolerated, the dose is sequentially increased every two weeks. Parents or caregivers also feed their child a pre-measured amount of peanut powder daily at home. Without OIT, research shows only 20 percent of children with peanut allergies outgrow the allergy over time. With the therapy, however, that chance climbs as high as 86 percent for Jackson.
“Our immune systems are more adaptable when we are younger because we are still growing and learning,” Coleen explained. “When a child is exposed to allergens earlier, there is a greater chance for their immune system to grow and potentially tolerate peanuts over time.”
Over the next 9-12 months, Dr. Mustafa explained he would work closely with the family to slowly increase Jackson’s daily dose of peanut protein until he is at the point where he can tolerate an amount that most people would normally eat and incorporate it into his diet as his parents see fit.
“We want to give these children the chance to outgrow this allergy while they have the opportunity,” Dr. Mustafa said.
Initially, Coleen was very anxious about starting the therapy. After the first couple of doses, however, she said her perspective shifted a bit.
“Once I started doing it, it helped me to become a little less apprehensive about giving [Jackson] something that is considered ‘life threatening,’” Coleen said. “That’s how I thought of it when I first started giving my child this food.”
Another element that put Coleen’s mind at ease is Dr. Mustafa’s own experience with serious allergies. His young son lives with allergies; knowing he goes through these situations in both his professional and personal life strengthens the trust he builds with his patients.
“The way Dr. Mustafa talks about the therapy process makes it clear that he knows exactly what he’s talking about,” Coleen said. “You feel very comfortable trusting him.”
“Every family has different goals, everyone comes from a different place, and health care is not ‘one size fits all,’” Dr. Mustafa said. “With oral immunotherapy, there is no ‘one size fits all’ management plan for food allergies. In that way, having family members with allergies and chronic health conditions helps me be a better clinician.”